Tuberculosis and comorbidities
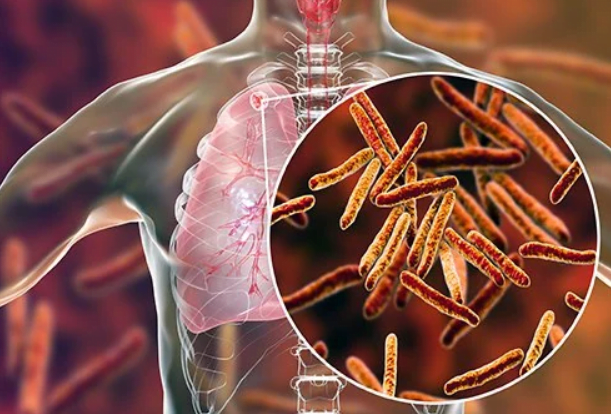
Globally, tuberculosis (TB) remains one of the leading causes of death due to a single infectious agent. The main TB comorbidities and health-related risk factors include human immunodeficiency virus (HIV), disorders due to the use of alcohol, undernutrition, tobacco smoking, diabetes mellitus, mental disorders, silicosis and viral hepatitis. Addressing health-related risk factors and comorbidities among people with TB is essential for ending the TB epidemic. To achieve this, care should be organized around the end user, rather than around the respective diseases.
There is substantial global commitment to address TB and comorbidities collaboratively.
Integrated patient-centred care and prevention for TB, including for HIV-associated TB and
other comorbidities are key components of pillar one of the End TB Strategy. The importance of integrated people-centred services is reiterated by the political declarations of the respective United Nations high-level meetings (UN HLMs) on the fight against TB, on noncommunicable diseases (NCDs), on HIV and AIDS, and on universal health coverage (UHC).
Although global guidance on interventions to address TB and comorbidities exists, its uptake
has been variable. Therefore, the World Health Organization (WHO), in consultation with key stakeholders, has developed a Framework for collaborative action on TB and comorbidities to enhance the response to TB and comorbidities, contributing towards addressing multimorbidity as part of people-centred care. The Framework is complementary to, and intended to be used in conjunction with, WHO guidelines on the prevention, screening, diagnosis and treatment of TB and key comorbidities. The strategies presented in this document endeavour to build strong collaboration across health programmes, affected communities, civil society, public and private health sectors, non-health actors and other stakeholders involved in health and social protection for people with TB and comorbidities.
This Framework is intended for use by people working in ministries of health, particularly in
national programmes or departments responsible for TB, HIV, NCDs, primary health care, tobacco cessation, undernutrition and substance use. It is also targeted at relevant line-ministries, policy-makers, international technical and funding organizations, researchers, nongovernmental and civil society organizations. In addition, it is intended for primary care workers, specialist health practitioners, and community health workers who support the response to TB and comorbidities both in the public and private sectors.
The Framework is organized in the following five sections, each of which lists key activities for scaling up collaborative action on TB and comorbidities. These sections are: (A) Strengthen governance and accountability for collaborative action; (B) Conduct an analysis of access to quality services for TB and comorbidities; (C) Coordinate planning and resource mobilization for collaborative action; (D) Implement and scale up people-centred services for TB and comorbidities; and (E) Strengthen monitoring, evaluation and research.
Summary of the Framework for collaborative action on TB and comorbidities
Strengthen governance and accountability for collaborative action
A.1 Strengthen political commitment, coordination and accountability for collaborative action on TB and comorbidities
A.2 Support financing and legislation that promote people-centred care
A.3 Ensure meaningful engagement of civil society and affected communities at all stages of planning, implementation, monitoring and evaluation
Conduct an analysis of access to quality services for TB and comorbidities
B.1 Assess the joint burden of TB and comorbidities
B.2 Determine access to services and the financial burden for people with TB and comorbidities
B.3 Map health service delivery for TB and comorbidities
B.4 Identify gaps in services and conduct root cause analysis
Coordinate planning and resource mobilization for collaborative action
C.1 Identify priority comorbidities and interventions
C.2 Define and reorient models of care for TB and comorbidities towards people-centred services, primary health care and universal health coverage
C.3 Conduct collaborative planning and budgeting to scale up people-centred services for TB and comorbidities
C.4 Align advocacy and communication across health programmes Implement and scale up people-centred services for TB and comorbidities
D.1 Jointly develop policies, guidelines and procedures for collaborative action on TB and comorbidities
D.2 Mobilize a qualified multidisciplinary workforce, including among private providers and non-health sectors for collaborative action
D.3 Ensure access to essential medicines, vaccines, diagnostics and health technologies for TB and comorbidities
D.4 Engage civil society and communities affected by TB and comorbidities in refining and delivering people-centred services
D.5 Optimize access to social protection to prevent financial hardship due to TB and comorbidities
D.6 Facilitate uptake of digital technologies to deliver health and social protection services across Programmes
D.7 Introduce phased scale-up of people-centred services for TB and comorbidities
Strengthen monitoring, evaluation and research
E.1 Adopt indicators and set targets for collaborative action on TB and comorbidities
E.2 Strengthen surveillance for comorbidities among people with TB, and surveillance for TB among people with comorbidities and health-related risk factors in accordance with WHO recommendations
E.3 Introduce and scale up monitoring and evaluation of collaborative action on TB and comorbidities at all levels
E.4 Conduct joint reviews of quality and coverage of services to inform programming
E.5 Conduct operational and implementation research to inform policy, programming and service delivery
Source: World Health Organisation